Blast & Ballistic Wounds (Conflict & Disaster Care)

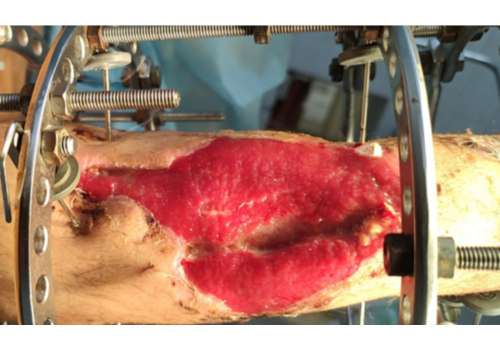
High-energy injuries from blast and ballistic trauma create not only a wound channel but wide contusion/commotion zones with microvascular collapse, evolving necrosis, and heavy contamination—common in conflict zones and mass-casualty/disaster settings (often called combat or war wounds). LINLINE’s MULTILINE™ platform uses a two-step laser pathway to meet this challenge: precise Er:YAG ablative sanitation to clean and vitalize the wound bed, followed by RecoSMA® field therapy to accelerate reparative regeneration with minimal collateral damage.
Why this method is different
- Layer-controlled debridement (cool, precise). At 2.94 µm, Er:YAG removes necrosis, slough, fibrin, debris, and biofilm in ≤ ~100 μm layers under direct vision—without deep thermal injury. Appearance of capillary “blood-dew” signals viable tissue and helps prevent over-excision.
- Non-thermal deep stimulation (RecoSMA®). After sanitation, the SMA module creates surface micro-events that launch acoustic waves into the dermis/subdermis. Their interference pattern improves microcirculation, drives granulation, and supports functional tissue replacement—without heating or new fibrosis.
- Built for contaminated wounds. Combining sterilizing ablation with regenerative stimulation is especially valuable when wounds are colonized/infected (including resistant flora) and standard measures underperform.
Indications in conflict, disaster, and austere care
- Blast and fragmentation injuries (shrapnel)
- Ballistic gunshot wounds
- Thermal and mixed blast-thermal injuries
- Contaminated, infected, or dehisced wounds after emergency surgery
- Chronic non-healing defects during prolonged care (e.g., neurotrophic/diabetic/venous ulcers)
Goal: create a clean, vital bed quickly, restart orderly repair, and move to secondary sutures or grafting sooner—while limiting long-term scarring and functional loss.
The two-step protocol
1) Er:YAG ablative sanitation (laser debridement)
- Actions: removes non-viable tissue and biofilm, reduces microbial load independent of antibiotic sensitivity.
- Technique: short-pulse, layer-by-layer ablation until blood-dew; repeat early in care as needed.
2) RecoSMA® regenerative field therapy
- Actions: stimulates granulation and neo-epithelialization, improves perfusion, and counteracts fibrosis in and around the wound.
- Coverage: treat the wound surface and extend 2-3 cm onto perilesional skin to normalize the microenvironment.
Dressings & adjuncts: simple sterile dressings; integrate with compression/off-loading, antibiotics, VAC/NPWT, and reconstructive steps per standard protocols.
What teams see in practice (typical patterns)
- Post-traumatic/ballistic wounds & dehiscence: daily sanitation + staged RecoSMA® often prepares for secondary sutures in ~3–14 days; full closure in weeks, depending on defect size and systemic status.
- Infected/colonized wounds (including resistant flora): granulation within days and progressive size reduction; epithelialization over weeks–months in large defects.
- Pain & function: frequent pain reduction and improved trophic status as the course advances.
(Outcomes vary with perfusion, load management, contamination level, and systemic care—this laser pathway is an adjunct that shortens the road to a clean, closing wound.)
Field & austere deployment advantages
- One platform, multiple roles: precise debridement, regeneration (RecoSMA®), and a laser scalpel mode with adjustable coagulation for surgical tasks.
- Logistics-ready: operates from a 220 V, ~3 kW generator—suitable for field hospitals, mobile units, and disaster response.
- Fast sessions: typical wound passes 5–30 minutes depending on area/depth; local anesthesia often unnecessary for Er:YAG sanitation.
Where it fits in the trauma pathway
- Damage control: hemorrhage control, resuscitation, fracture stabilization, gross debridement.
- Laser step: Er:YAG sanitation to achieve a truly clean, vital surface; RecoSMA® to jump-start granulation and stabilize the bed.
- Definitive closure: secondary sutures/grafts when ready; continue RecoSMA® to reduce scar stiffness and support function during maturation.
- remain essential; the laser pathway is an adjunct, not a replacement.
Benefits at a glance
For patients
- Cleaner wounds sooner, less pain, faster path to closure.
- Lower scar burden thanks to non-thermal sanitation and regenerative stimulation.
For medical teams
- Reproducible endpoints: blood-dew confirms viability; granulation/epithelial march confirm progress.
- Logistics-friendly: one generator-powered unit that debrides, regenerates, cuts, and coagulates.
- Plays well with others: integrates with VAC/NPWT, compression, antibiotics, and reconstructive surgery.
Key takeaway
Blast & Ballistic Wounds demand precision and speed. By pairing Er:YAG ablative sanitation with RecoSMA® regenerative stimulation on the MULTILINE™ platform, clinicians can clean precisely, stimulate deeply, and close sooner—in austere field conditions or advanced centers—while preserving viable tissue and long-term function.









 06.10.2025
06.10.2025